Butalbital/acetaminophen, sold under the brand name Butapap among others, is a combination medication used to treat tension headaches and migraine headaches.
It contains butalbital, a barbiturate and paracetamol (acetaminophen), an analgesic. Versions also containing caffeine are sold under the brand name Fioricet among others. It is taken by mouth. The combination is also sold with codeine.
The most common side effects include sleepiness, dizziness, trouble breathing, and abdominal pain. Other severe side effects may include liver problems, confusion, addiction, and allergic reactions.

What is Oblong Blue Fioricet ?
Frequent use may result in medication overuse headache. Barbiturate withdrawal may occur if rapidly stopped following long term use. Use is not generally recommended during pregnancy or breastfeeding.
The combination was approved for medical use in the United States in 1984. It is available as a generic medication.
In 2020, the combination butalbital/acetaminophen/caffeine was the 201st most commonly prescribed medication in the United States, with more than 2 million prescriptions.
In the United States it is a schedule III controlled substance in some states but not federally. It is banned in a number of European countries.
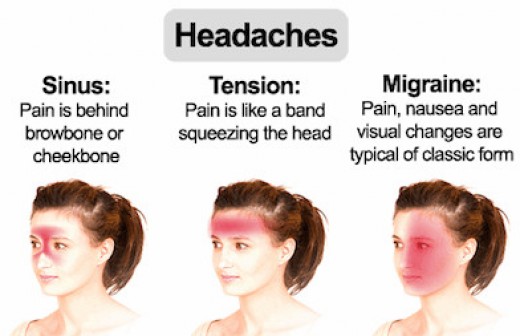
What is A Headache ?
Headache is pain in any region of the head. Headaches may occur on one or both sides of the head, be isolated to a certain location, radiate across the head from one point, or have a viselike quality.
A headache may appear as a sharp pain, a throbbing sensation or a dull ache. Headaches can develop gradually or suddenly, and may last from less than an hour to several days.
Primary headaches
A primary headache is caused by overactivity of or problems with pain-sensitive structures in your head. A primary headache isn’t a symptom of an underlying disease.
Chemical activity in your brain, the nerves or blood vessels surrounding your skull, or the muscles of your head and neck (or some combination of these factors) can play a role in primary headaches. Some people may also carry genes that make them more likely to develop such headaches.
The most common primary headaches are:
-
- Cluster headache
- Migraine
- Migraine with aura
- Tension headache
- Trigeminal autonomic cephalalgia (TAC), such as cluster headache and paroxysmal hemicrania
A few headache patterns also are generally considered types of primary headache, but are less common. These headaches have distinct features, such as an unusual duration or pain associated with a certain activity.
Although generally considered primary, each could be a symptom of an underlying disease. They include:
-
- Chronic daily headaches (for example, chronic migraine, chronic tension-type headache, or hemicranias continua)
- Cough headaches
- Exercise headaches
- Sex headaches
Some primary headaches can be triggered by lifestyle factors, including:
-
- Alcohol, particularly red wine
- Certain foods, such as processed meats that contain nitrates
- Changes in sleep or lack of sleep
- Poor posture
- Skipped meals
- Stress
Secondary Headaches
A secondary headache is a symptom of a disease that can activate the pain-sensitive nerves of the head. Any number of conditions — varying greatly in severity — may cause secondary headaches.
Possible causes of secondary headaches include:
-
- Acute sinusitis
- Arterial tears (carotid or vertebral dissections)
- Blood clot (venous thrombosis) within the brain — separate from stroke
- Brain aneurysm
- Brain AVM (arteriovenous malformation)
- Brain tumor
- Carbon monoxide poisoning
- Chiari malformation (structural problem at the base of your skull)
- Concussion
- Coronavirus disease 2019 (COVID-19)
- Dehydration (when the body doesn’t have enough water and other fluids to work as it should)
- Dental problems
- Ear infection (middle ear)
- Encephalitis (brain inflammation)
- Giant cell arteritis (inflammation of the lining of the arteries)
- Glaucoma (acute angle closure glaucoma)
- Hangovers
- High blood pressure (hypertension)
- Influenza (flu) and other febrile (fever) illnesses
- Intracranial hematoma
- Medications to treat other disorders
- Meningitis
- Monosodium glutamate (MSG)
- Overuse of pain medication
- Panic attacks and panic disorder
- Persistent post-concussive symptoms (Post-concussion syndrome)
- Pressure from tight headgear, such as a helmet or goggles
- Pseudotumor cerebri (idiopathic intracranial hypertension)
- Stroke
- Toxoplasmosis
- Trigeminal neuralgia (as well as other neuralgias, all involving irritation of certain nerves connecting the face and brain)
Some Types of Secondary Headaches Include:
-
- Ice cream headaches (commonly called brain freeze)
- Medication overuse headaches (caused by overuse of pain medication)
- Sinus headaches (caused by inflammation and congestion in sinus cavities)
- Spinal headaches (caused by low pressure or volume of cerebrospinal fluid, possibly the result of spontaneous cerebrospinal fluid leak, spinal tap or spinal anesthesia)
- Thunderclap headaches (a group of disorders that involves sudden, severe headaches with multiple causes)